RIO DE JANEIRO, BRAZIL – The National Health Regulatory Agency (ANVISA) issued an alert on Monday, December 7th, about an ongoing investigation of a possible first positive case in the country of Candida auris, a drug-resistant fungus responsible for hospital infections that has become one of the most feared in the world.
In its alert, ANVISA stated that Candida auris (C. auris) “is an emerging fungus that represents a serious threat to public health.”
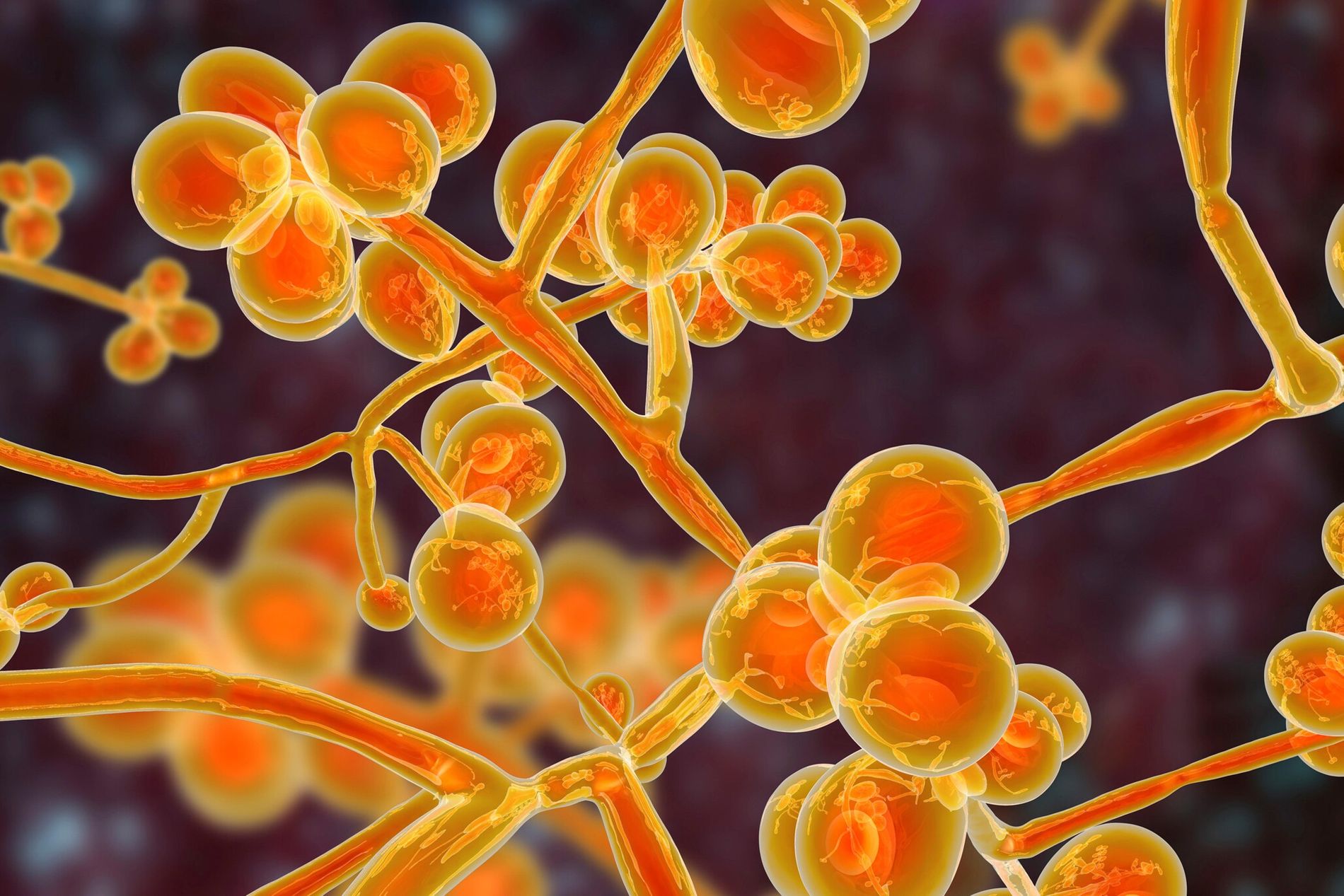
C. auris infection is drug-resistant and can be fatal. Worldwide, it is estimated that C. auris invasive fungal infections have led to the death of between 30% and 60% of patients.
According to ANVISA’s alert, the fungus was identified in a “catheter tip sample of a patient admitted to an adult ICU in a hospital in the State of Bahia”. The sample was analyzed by the Central Public Health Laboratory in Salvador, and by the Laboratory of the Clínicas Hospital of São Paulo Medical School.
ANVISA states that the sample is still submitted to “phenotypic analysis (to determine its sensitivity and resistance profile)” and “genetic sequencing of the microorganism (gold standard)” until the case is officially confirmed.
Given the suspicion, ANVISA recommended the strengthening of laboratory surveillance of the fungus in all health services in the country, among other control and prevention measures to avert an outbreak.
The fungus was first identified in 2009 in the ear canal of a patient in Japan. Since then, there have been cases identified in countries around the world.
In 2016, PAHO, the World Health Organization’s Latin American arm, issued an alert recommending the adoption of prevention and control measures because of fungus-related outbreaks in the region. The first outbreak in the region occurred in Venezuela, between 2012 and 2013, affecting 18 patients.
In addition, C. auris is often confused with other infections, leading to incorrect treatment.
“C. auris survives in hospital environments and therefore cleanliness is critical to control it. The detection (of fungus) can be a serious issue for both patients and the hospital, since control can be difficult,” explained Dr. Elaine Cloutman-Green, an infection control specialist and professor at University College London (UCL).
Not all hospitals identify C. auris the same way. Sometimes the fungus is confused with other fungal infections, such as the common candidiasis.
In 2017, a research study published by Alessandro Pasqualotto, from Porto Alegre’s Santa Casa de Misericórdia, analyzed 130 laboratories of reference medical centers in Latin America and found that only 10% of them are capable of detecting invasive fungal diseases according to European standards.
According to ANVISA, the 2016 Cartagena outbreak in Colombia is an illustration of how the microorganism is difficult to detect. Five cases of infection were identified as three different fungi until a more modern method of analysis correctly diagnosed the pathogen as C. auris.
Furthermore, C. auris is very resistant and can survive on surfaces for a long time. It is also not possible to eliminate it using the most common detergents and disinfectants. It is therefore important to use the appropriate hospital cleaning chemicals, particularly if there is an outbreak.
In an alert issued in 2017, ANVISA explained that the most accurate way of fungus transmission within a health unit is unclear. Studies suggest that this can occur through contact with contaminated surfaces or equipment and from person to person.
The largest outbreak linked to C. auris occurred in 2015 in London, with 22 infected patients and another 28 quarantined.
Resistance to common antifungals such as fluconazole was observed in most C. auris strains found in patients. This means that these drugs do not work to fight C. auris. As a result, less common fungicidal drugs have been used to treat these infections, but C. auris has also developed resistance to them.
“There is a record of resistance to azoles, echinocandins, and even polyenes, such as amphotericin B. This means that the fungus can be resistant to the three main classes of drugs available to treat systemic fungal infections,” explained epidemiologist and microbiologist Alison Chaves on Twitter.
DNA analysis also shows that antifungal resistance genes present in C. auris have passed on to other species of fungus, such as Candida albicans (C. albicans), one of the main causes of candidiasis (a common disease that can affect the skin, nails and genital organs, and is relatively easy to treat).

