RIO DE JANEIRO, BRAZIL – Among people diagnosed with depression, some suffer from a form that is difficult to treat: resistant depression. In this case, the patient usually performs two types of treatments correctly and does not get better.
For example, the physiotherapist Cláudio Andrade de Oliveira (46) was diagnosed with the disease during the pandemic. He was already taking two medications in the morning and one in the evening. But as Covid-19 spread worldwide, his condition worsened, and the doctor made the diagnosis.
Claudio has suffered from mental disorders since his teenage years. By 18, he was taking anxiolytics and even had severe depressive crises while living in the United States in 2004, where he could not afford private treatment.
In 2009, he returned to Brazil and sought treatment again, but during the Covid event, his mental health deteriorated: he only stayed down and could no longer work. “The psychiatrist increased the medication as much as possible, and sometimes he changed it, but nothing solved the problem; I continued to suffer from extreme depression,” he said.
There was no improvement until January of this year after she tried treatment with ketamine, which had an effect. “To this day, I don’t feel that anxiety and extreme anxiety anymore; I feel the normal worries that everyone has,” he said.
Today, the specialist still monitors him, but he has been discharged from the treatment he underwent earlier this year. “I’ve been discharged after six infusions of ketamine,” he says.
WHAT IS KETAMINE?
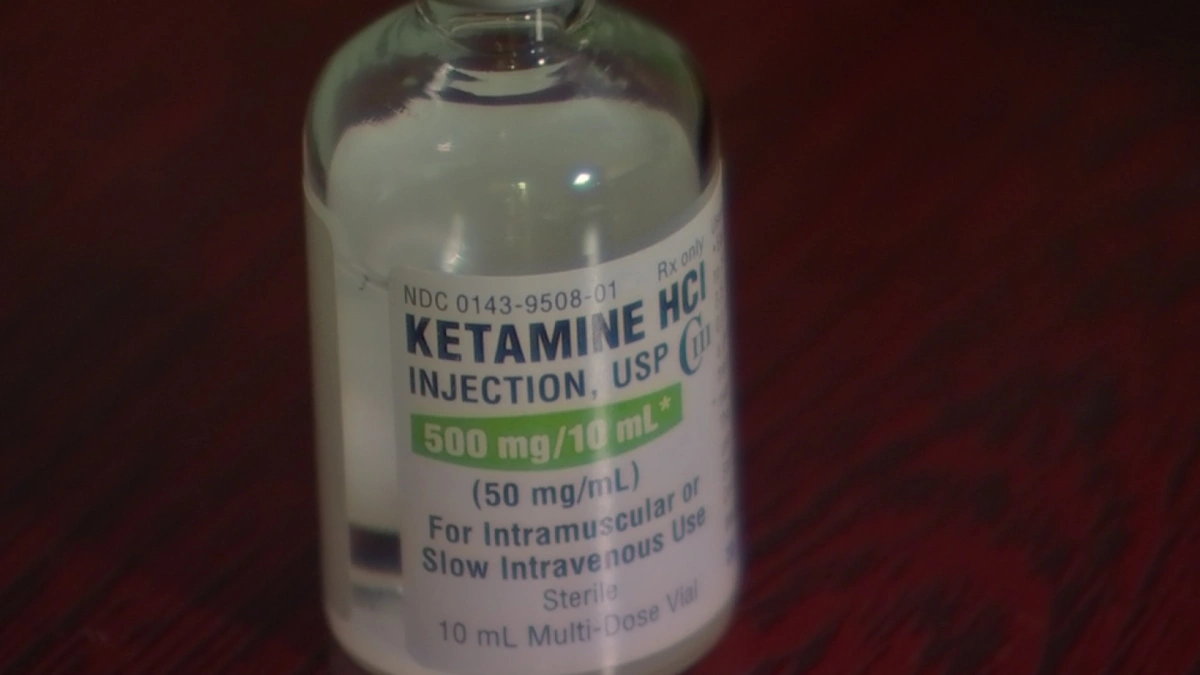
Ketamine is a hospital anesthetic used for sedation in several countries, including Brazil, but it is also a new alternative for treating resistant depression. In Brazil, it was approved in November 2020 by Anvisa (National Health Inspectorate) as a drug for this type of mental disorder.
For this purpose, it must be administered exclusively in a hospital or specialized clinic and the presence of a healthcare professional, according to the agency. It is used intravenously or as a nasal spray but is not yet available at SUS.
Although the results of studies conducted with ketamine are encouraging, caution is needed when prescribing it, according to Alexander Moreira de Almeida, associate professor of psychiatry at the UFJF (Federal University of Juiz de Fora Medical School) and coordinator of the PTA (Program for Anxiety Disorders) at the same institution.
“It is a drug that has recently come on the market, and its effects are more rapid, but nothing is known about its efficacy and safety in long-term use,” Almeida warns. “There has been a strong promotional campaign for this drug, but caution is advised,” he says.
After administration, the substance enters the brain, triggers a process of neuron reattachment, and leaves the body after about 20 hours. This way, the cells begin to “talk” to each other and connect better. As a result, the areas affected by the disease function better again, and patients notice an improvement in depressive symptoms.
However, there are side effects. “The adverse effects of ketamine occur during the infusion and are potentially severe and even fatal, so an anesthesiologist must accompany the procedure and be in a hospital where a cardiogram, oximeter, and blood pressure are measured every 10 minutes, says Tiago Gil, anesthesiologist, and founder of the Ketamine Center, an active member of ASKP3 (American Society of Ketamine Physicians, Psychotherapists & Practitioners) and volunteer researcher at IPq-HCFMUSP (Psychiatric Institute at the University of São Paulo Medical School Hospital).
The most common recurrent side effects include:
- Increased blood pressure;
- Increased heart rate;
- General anesthesia with respiratory arrest;
- Nausea and vomiting;
- Dissociation (an altered state of awareness of the environment).
According to the anesthesiologist, all symptoms disappear within 24 hours after the infusion.
Physician Amanda Rocha*, 37, who also suffers from resistant depression, responded well to treatment with the substance. “It’s a milestone in my life because I feel better and have almost no side effects, just dissociation, nausea, and dizziness, but they go away quickly,” she says.
She was diagnosed about 20 years ago, and at first, it was a mild condition that she treated only with an antidepressant. She responded to the treatment for two years, but it stopped working.
Medications were adjusted, and others added, but the illness fluctuated. Amanda also participated in electroconvulsive therapy, but it didn’t significantly improve. “I was never able to stop the medication,” she says.
In 2020, however, she also discovered ketamine, and this time she had good results. “I did six sessions using it in the vein, but since it’s a relatively new drug, even health professionals have little knowledge and are reluctant to refer the patient to this type of treatment,” Rocha says.
Today, she says she is doing much better but continues to have sporadic sessions.
Are there other treatment options for resistant depression?
Resistant depression is when a patient’s condition does not improve even after treatment with two different classes of antidepressants at appropriate doses and for the proper duration.
“The likelihood that the third medication will respond decreases sharply. This was evident in a study from the United Kingdom that assessed the quality of responses to the antidepressant at the first, second, third, and fourth doses,” says Tiago Gil.
Psychiatrist Raissa de Alexandria, from HULW-UFPB (Hospital Universitário Lauro Wanderley da Universidade Federal da Paraíba), which is affiliated with the Ebserh network, explains that resistant depression is one of the most severe syndromes.
“They are stable conditions that can become chronic and cause more serious symptoms, such as suicidal thoughts. But that can happen even with a non-refractory picture,” he cautions.
According to the specialist, 10 to 15% of patients with depression suffer from refractory depression.
In the case of refractory depression, transcranial magnetic stimulation, also used to treat various other psychiatric disorders, can be used in addition to conventional medications in conjunction with therapy.
Electroconvulsive therapy is another option for this pathology and, according to experts, is an essential tool that can save lives.
Psychotherapy is also essential. “There are studies that show that patients do better if they do cognitive behavioral therapy in addition to taking antidepressants,” says Alexander Moreira de Almeida.
In addition to antidepressants, other medications can work together to enhance treatment.
Regardless of the treatment, the patient must follow the guidelines closely. “It’s important for the patient to adhere to treatment appropriately. They often forget to take their medication for a few days, don’t take it regularly, or use other substances such as alcohol or drugs that can interfere with the effects of the medication,” Alexandria warns.
It’s difficult to talk about a cure for mental health disorders. In these cases, once treatment has achieved its goal, the person returns to everyday life, just as before the illness. However, this does not mean that they will not relapse at some point.
That’s why the patient needs to remain physically active, maintain social contacts, and pursue a hobby that makes them feel good, even after the physician-ordered medication suspension.
*At the request of the character, her name has been changed.

