RIO DE JANEIRO, BRAZIL – (by Ester Lázaro Lázaro*) Since the outbreak of the Covid-19 pandemic, comments about concerns that SARS-CoV-2 would mutate into a more aggressive strain have been commonplace. For many, the virus was seen as an entity capable of making decisions to ensure its permanence among us.
In fact, viruses do not make any decisions. As soon as they infect a cell, they begin to multiply almost automatically, a process that entails copying their genetic information. During the copying process, errors often occur, which despite not often having any impact, occasionally produce changes in some of the amino acids that make up the virus’s proteins. As a result, the three-dimensional structure of these macromolecules can be altered, and with it the virus’ properties.
More SARS-CoV-2 strains than ever before
If viruses are constantly mutating, why is it that there seem to be more SARS-CoV-2 strains than ever before? Because we’re placing obstacles in the way of its transmission.
Things were very different at the start of the pandemic. We were all susceptible to SARS-CoV-2, there was a severe shortage of protective equipment to prevent infection, and we were unaware of the best measures to prevent it. The result was that the virus was virtually free to infect us, and the slightly more contagious strains had little advantage over the rest.
A year into the pandemic, the situation has changed. Many people have already been infected and now possess antibodies to the virus. We have access to masks and we have learned that the virus is transmitted by aerosols, which allows us to prevent contagion with good ventilation. Finally, a vaccination process has been initiated and in some countries it has already covered a large part of the population.
In short, we are making it increasingly difficult for the virus. And a direct consequence is that, under pressure, the most transmissible strains have an advantage over the rest and may become the majority.
Increased infection does not mean increased mortality
There are several ways in which a virus can enhance its transmission. Among them is by increasing its capacity to interact with the cellular receptor, the molecule that allows it to enter the cell. Another, in populations with a large number of individuals who have already been infected, is to prevent being recognized by antibodies. The good news is that increased infection capacity is not typically associated with increased mortality. It does not matter for the virus, because if an infected individual dies early or develops very severe symptoms, he or she will be less likely to spread it.
The SARS-CoV-2 strains that are currently causing greatest concern, due to the speed with which they are spreading, are the British, South African and Brazilian variants, named after the places where they were first detected. According to the most widely accepted nomenclature for the classification of virus strains, these variants are the B.1.1.7 (British), B.1.351 (South African) and P.1 (Brazilian).
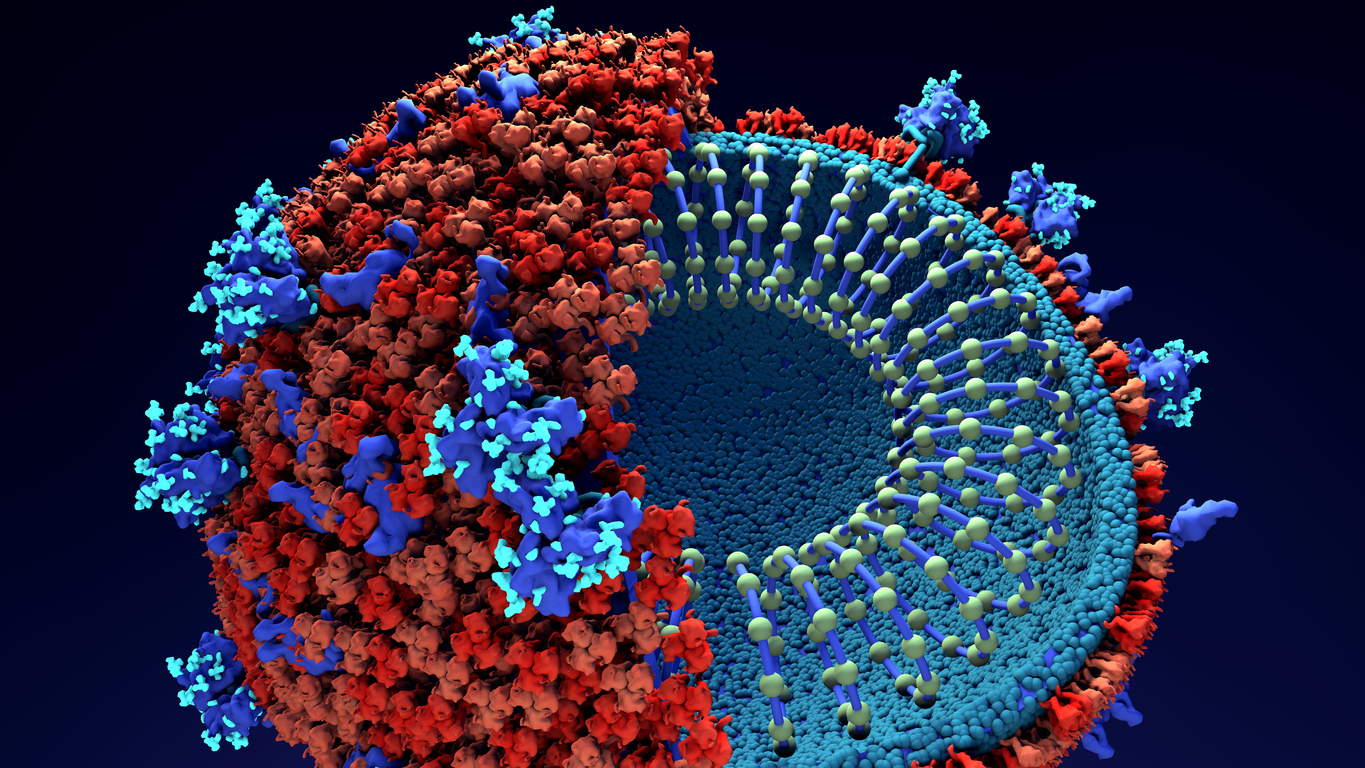
Each of these strains contains a particular set of mutations, some of which are coincidental. Of these, the most worrisome are those located in the S or spicule protein, which interacts with the cellular receptor and towards which much of the immune response is directed. We still do not know much about these mutations, but we are beginning to see some clues. However, one should bear in mind that the potential advantages of a viral variant are usually not the result of a single mutation, but rather of a combination of several.
Which mutations do the new SARS-CoV-2 strains contain?
The N501Y mutation, which replaces the amino acid asparagine found on the spicule at position 501 with a tyrosine, is common to all three strains and produces a change in this protein’s structure that increases its ability to bind to the cellular receptor. It is as if we were cutting a key so that it would better fit into its lock.
The E484K mutation, present in the Brazilian and South African variants, has also been identified in the spicule. Everything suggests that, in addition to favoring binding to the receptor, it could lead to the virus being more difficult to neutralize by antibodies, thus increasing reinfections or decreasing the efficacy of vaccines.
The finding of these mutations in viral genomes isolated in different parts of the world, and belonging to different evolutionary strains, is another indicator of their potential advantage over viruses that do not contain them.
Another interesting mutation is the deletion of amino acids at positions 69 and 70 of the spicule. The mutation, which was also detected in viruses isolated from massive infections that occurred in several mink farms a few months ago in the Netherlands and Denmark, illustrates how the spread of the virus in species other than humans can favor the emergence of new and more dangerous strains for humans. In particular, this mutation seems to work in synergy with the previously described N501Y, further increasing affinity with the receptor.
Is the British strain more lethal?
In recent days, doubts have emerged as to whether or not the British variant is more lethal in elderly people. The fact is that any more transmissible variant will likely increase the number of deaths, not only because of a higher number of infections, but also because of increased difficulties in treating the sick.
There is also great concern that the circulation of these strains will impact the efficacy of vaccines or the frequency of reinfection, as has been discussed in the case of the South African and Brazilian strains. The fact is that the majority of studies on the effect of antibodies on these viruses have been performed in in vitro tests, which do not consider the complex immune response produced in an organism.
If the reduced efficacy of vaccines on these strains were to be confirmed, it would not be a debacle. It would simply mean that vaccines would have to be periodically updated according to the strains in circulation at the time. This is common with the influenza virus, which may even be much more feasible with the new RNA vaccines. Once again we are witnessing how scientific research is our best ally for survival.
*Ester Lázaro Lázaro is a Research Scientist at Public Research Organizations. Specialized in virus evolution, Astrobiology Center (INTA-CSIC).
Source: Infobae

