RIO DE JANEIRO, BRAZIL – Viruses are tiny, limited to the bare essentials, and whether or not they survive at all is controversial at best. They dock to cells, introduce their genetic material into the cell and then use the cell mechanism to multiply.
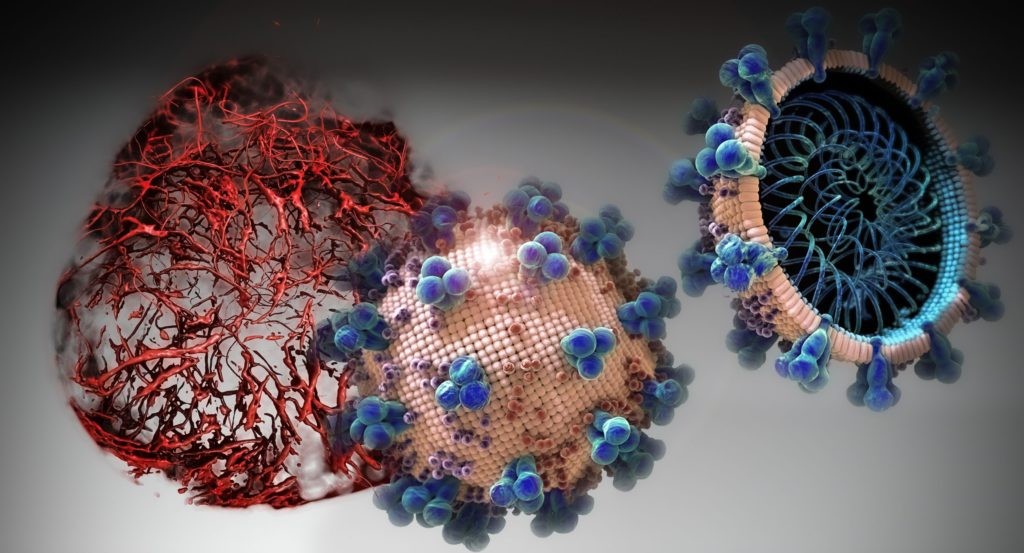
The novel coronavirus is no exception. It is a tiny sphere whose surface is covered with a kind of blunt thorns, the so-called spikes, which under the microscope seem like a kind of crown – hence its name. Inside the sphere is – after all – the largest genome known from a single-stranded RNA virus.
In addition to coronaviruses, this viral group also includes influenza and HI viruses.
But this tiny virus has successfully managed to paralyze the world. Not everywhere, not completely, but so thoroughly that even seismologists are said to be able to determine it: The earth’s surface is said to vibrate less due to limited human activity.
It has succeeded in doing this because of a very special combination of properties that its predecessors did not possess.
It can be easily transmitted from person to person, which was or is what the pathogens of SARS were or are to a far lesser extent, which (in percentage terms) caused considerably more deaths. Nevertheless, it causes severe respiratory disease in a substantial proportion of those infected, from which a certain (currently still unclear) percentage of patients die.
This in turn distinguishes it from other coronaviruses, which have been present in humans for a long time and cause mild colds.
Easy to activate
What makes it so easily transmissible? We don’t yet know exactly, but researchers have identified a first possible clue. The virus cannot simply dock anywhere on a cell, but only at specific spots where the so-called ACE2 receptors (angiotensin-converting enzyme-2 receptors) are present, the same ones that the SARS viruses use.
These receptors are much more common in the lower airways than in the upper airways and fit into the receptor binding spot on the spike protein in the virus like a keyhole to a key.
However, in order to unlock the cell and introduce its genetic material into it, the virus must first be activated, as Silke Stertz from the University of Zurich explains. This is done by cutting the spike protein at a specific location by an enzyme of the host cell, a protease.
The SARS pathogen needs a very specific, not too frequently occuring protease for this, says Stertz. In contrast, Sars-CoV-2 is much more flexible and can use a protease that is present in many different cell types.
Stertz now believes that it can be activated much more efficiently – and if there is a large amount of activated virus, the relatively rare ACE2 receptors in the nose and throat might also be enough to cause an infection. According to this theory, SARS, on the other hand, would be more difficult to spread because it would need to reach deeper into the lungs.
Bat and pangolin
In addition, the key and the “human” keyhole of the new coronavirus fit together particularly well. This is not the case with the closest known relative of Sars-CoV-2, a bat coronavirus called RaTG13.
Its blueprint for the spike protein is over 93 percent identical to that of sars-CoV-2. This makes it the one that is most similar to the novel coronavirus. However, not in every part of the gene: In pangolin animals seized in the Chinese province of Guangdong, scientists found coronaviruses whose receptor binding point was almost 98 percent identical to that of sars-CoV-2 – considerably more than that of the bat virus.
However, this high correlation only affected this spot. In terms of the remaining genome, the bat virus was still the most similar to the novel coronavirus.
The researchers speculate that the novel virus may have been created during a so-called recombination: when different coronaviruses (in this case the bat virus and the one found in psoriasis) infected the same cell, their genomes were disrupted and individual parts were recombined.
In fact, it is known that this process occurs again and again in coronaviruses and that new virus variants can also be formed.
It is also possible that the bat virus, or a closely related one, got into psoriasis and then adapted to its new hosts, whose ACE2 receptor is more similar to that of humans than that of the bat. However, the pangolin viruses lack the specific interface in the spike protein that distinguishes the novel coronavirus.
Is it evading inoculation?
Single-stranded RNA viruses are generally known for their genetic “mutability”. For various reasons, the enzymes responsible for duplicating the genetic material of these viruses are less precise than their equivalents in our genetic material.
As a result, tiny changes in the genetic material sequence, so-called mutations, occur again and again randomly distributed over the genome.
In the case of the influenza virus, this means that the vaccination has to be repeatedly adapted. This is because the accumulating mutations can also change the structure of the viruses which the immune system recognizes and against which it forms antibodies, the so-called antigen. With the novel coronavirus, however, there is so far no reason to be concerned by this, explains Silke Stertz.
First, coronaviruses change more slowly than influenza viruses, which mutate particularly rapidly. It is not entirely clear why. On the other hand, genetic changes must first establish themselves in the virus population. The vast majority of mutations have no consequences.
Their fate is subject to chance. If genetic changes damage the virus, they disappear from the population again because the affected virus cannot reproduce at all, or only to a limited extent.
To establish itself within a certain time, a mutation must be advantageous. In influenza viruses, for instance, mutations are those that cause changes in the antigen. These viruses have long been circulating in the human population.
When humans are infected, they are therefore very likely to come across antibodies that can neutralize the virus. However, changes in the antigen enable the affected viruses to evade the immune system, which leads to successful replication.
However, the novel coronavirus does not need to do this: the proportion of the world’s population that possesses antibodies against sars-CoV-2 is still small. Changes to the antigen do not benefit such a virus: viruses that possess them do not reproduce better or faster than those that remain unchanged because the immune system does not recognize either one or the other. Whether this will be the case in the long term will only become clear in the course of time, says Stertz.
Overall, however, the virus has already collected enough mutations to enable researchers to trace the spread of Sars-CoV-2 throughout the world by using different mutated viruses.
However, these mutations are small and randomly distributed over the genome. According to experts, the virus has, so far, neither undergone any fundamental changes, nor has it split into different viral strains that differ from each other in their properties.
However, in a publication that has not yet been scientifically reviewed, Chinese researchers describe mutations in the receptor binding domain (RBD) of several sequenced viruses that might make their binding to the cell more stable.
Such mutations might theoretically make the virus easier to be transmitted. However, they have not become widely accepted and have so far only been detected in a number of circulating viruses.

